Breast cancer patients in England will not be able to avail themselves of a life-prolonging drug after the country’s socialised healthcare system deemed it “too expensive”.
A drug that would prolong the lives of those with advanced breast cancer will not be made available to many patients in England after the country’s socialised healthcare system ruled it to be “too expensive”.
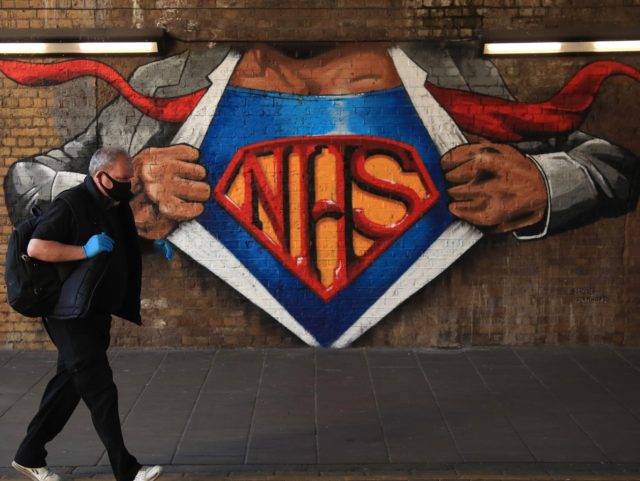
While the medicine known as Trodelvy will be made available publicly in Scotland, which manages its own state healthcare system, England’s National Institute for Health and Care Excellence (NICE) has decided it would be best that women south of the border not be able to avail themselves of the drug, claiming that it is not “cost-effective use of [National Health Service] resources”.
According to a report by The Telegraph, around 650 women in England would have benefitted from taking the drug, with one charity describing the decision as a “devastating blow”.
“Evidence shows Trodelvy can increase time before a patient’s disease progresses and, crucially, how long they live compared to being treated with chemotherapy,” said Delyth Morgan, who serves as Chief Executive of the charity Breast Cancer Now.
The charity head also took aim at the state healthcare system’s poor handling of cancer cases, saying that women deserve to gain access to such a drug.
“These women, who already face devastatingly poorer prognoses and limited treatment options, deserve the chance to benefit from this new treatment option,” the chief executive argued.
While seemingly extremely popular amongst the general public, the United Kingdom’s socialised healthcare system has a relatively poor track record when it comes to treating cancer cases effectively.
Wait times for treatment within the service are far from where the British government believes they should be, with a massive 98 per cent of NHS areas in England missing their wait-time targets for January of this year.
Meanwhile, survival rates for cancer patients within the system are low compared to other first-world counterparts, with less than three in five colon cancer patients surviving for five years or more post-diagnosis in Britain, compared to over two-thirds in Canada and 70.8 per cent in Australia.
This example appears to be representative of other variants of the illness, with a study by the London School of Hygiene and Tropical Medicine into cancer survival rates among 28 different nation-states regularly finding patients in the United Kingdom to have outcomes below the average.
However, it is not just cancer sufferers that the NHS is failing, with a review of maternal healthcare in one section of the socialised system finding that 300 babies died unnecessarily thanks to an unhealthy obsession with natural births.
“There were numerous opportunities for the system to wake up and realise that there was a problem at this trust,” said experienced midwife Donna Ockenden, who headed up the official investigation into the scandal, also commenting that she was “shocked and saddened” by her findings.
“There have been a number of occasions where families tried to be heard over many years and were silenced or ignored,” she lamented.
“We have seen families that have been split apart, families where relationships have been broken, cases of trauma and PTSD that have persisted for years after the event as well as terrible, terrible sadness.”
COMMENTS
Please let us know if you're having issues with commenting.